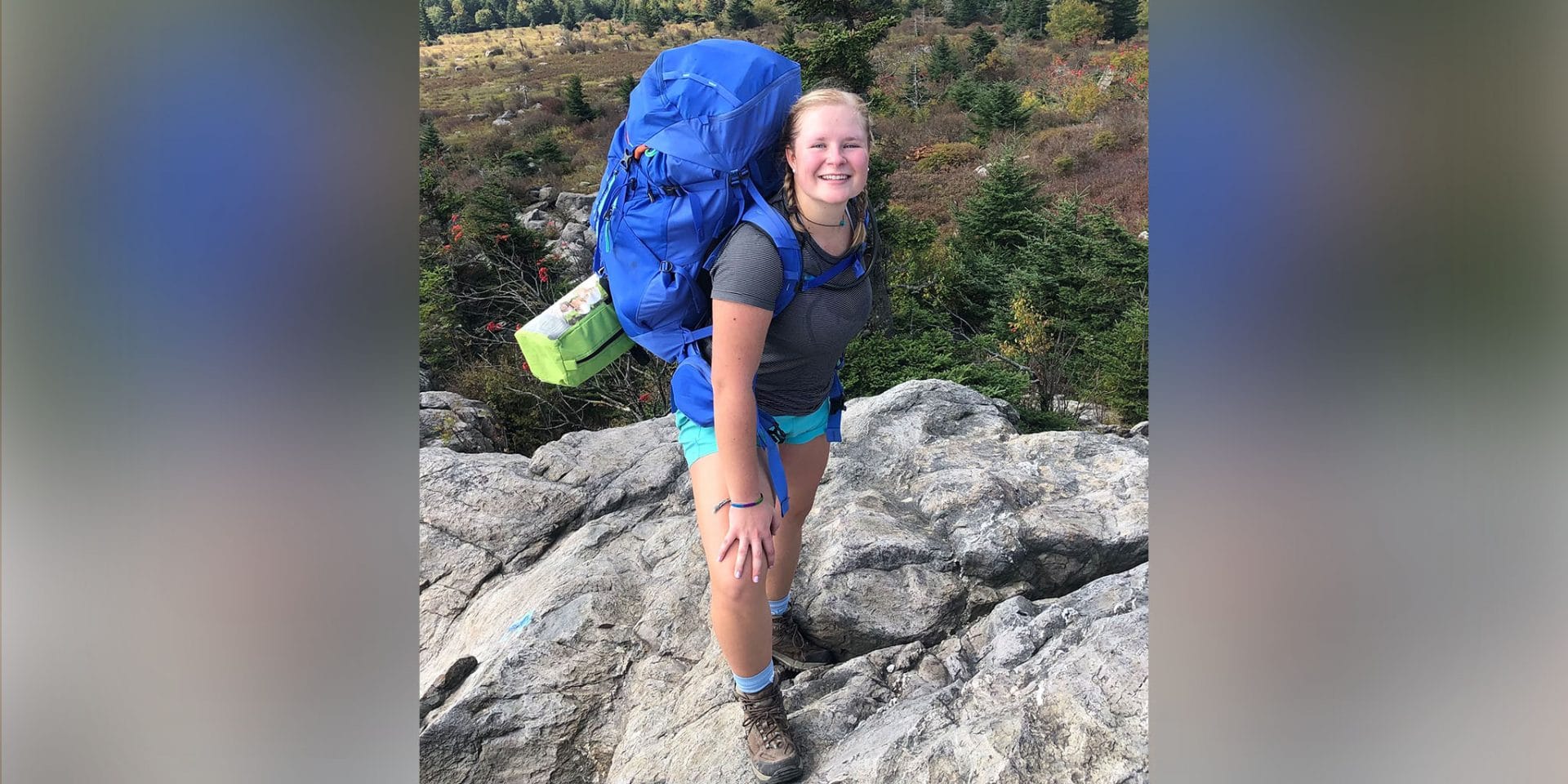
Frances Reed ’22 is an environmental health sciences major and chemistry minor at Carolina.
I can’t think of someone who better personifies Morehead-Cain’s mission—to sustain and enhance the excellence of the University of North Carolina at Chapel Hill—than my Morehead-Cain Mentor, Amir Barzin ’06.
Since the beginning of the COVID-19 pandemic in early 2020, Amir has been at the forefront of UNC–Chapel Hill’s and UNC Health’s response.
He’s led rapid testing as the incident commander for UNC Health’s Respiratory Diagnostic Center. As lead for COVID-19 testing, tracing, and care at Carolina, he’s provided vital health communications to the University and greater Triangle area throughout the crisis. He’s also served as medical director of the UNC Family Medicine Center at Chapel Hill and as chief resident physician of the UNC Department of Family Medicine.
Amir has now transitioned to become the medical director for virtual care services and the UNC Clinical Contact Center for UNC Health. But while these impressive roles indicate his incredible leadership within our community, they don’t come close to painting the full picture of the impact he’s had on all of those he serves and mentors, and with whom he collaborates.
As a physician and public health professional, he’s an expert at identifying needs—and then working relentlessly to fulfill those needs.
During one of our first mentoring conversations in September of 2020, as the University returned to online classes, he shared how deeply he empathized with the frustration and sadness of Carolina students for losing some of the best aspects of their college experience. I would’ve never imagined that, just a few months later, he’d win a grant to establish the Carolina Together Testing Program, a UNC testing initiative launched in January 2021.
He has worked day and night to get the lab running smoothly and to protect the health and safety of our community. By the following spring, the program was offering vaccinations to all students, faculty, and staff at the University. He enabled us get on track for a full return to campus.
Were it not for Amir, I might not be in Chapel Hill this fall, seeking to make up for lost time with friends and classmates. I’m continually inspired by his motivation of compassion and love for the Carolina and Chapel Hill communities.
Reflecting on his service, I see his long-term vision for investing in the future of Carolina. His sacrifice and leadership enables students like me to flourish. I hope to one day inspire others to reach within themselves to find and pursue what brings them fulfillment, just as Amir has done for me in discovering my passion for medicine.
I’ve long struggled with the tension of trying to fully devote myself to my commitments and interests, while also trying to discover a formulaic Nirvana of balance (sound familiar, anyone?). Amir taught me, however, that sometimes the right thing to do is to understand your limits while doing your best to invest in what is needed and will help others most. I’m learning that life has natural ebbs and flows, and that always trying to cultivate and live your perfect idea of balance can instigate another sort of exhaustion.
Amir and I also often talked about how, during times of crisis, we may not have time to go on long runs or play two hours of tennis, cook extravagant meals, sleep all eight hours, and spend the perfect amount of quality time with loved ones. Despite and perhaps even especially during stressful times, it’s important to seek out sources of joy rather than obsess over a fictional equation for success. He’s helped me realize that for me, that’s strengthening connections with people I hold dear in my communities.
I still don’t understand how Amir managed to find time to mentor and invest in me with the intention, commitment, and quality that comprise the trademark of his work. During his virtually no-sleep months in getting the student testing program established, I felt guilty at the thought that, by meeting with me, he was likely saying “no” to many other things that were asked of him. But he never made me feel less than a priority.
I’ve seen Amir’s example of intentionality and generosity in individual relationships cause a domino effect of inspired confidence and positive action in his communities. This has been one of the greatest lessons in leadership for me.
After establishing frameworks and systems to protect the University, Amir is taking a well-deserved parental leave to spend time with his newborn son, wife, and daughter. I don’t know that I always believe in absolute truths, but I’ve learned that people are the best investment. I hope to live out this truth with the fervent commitment that Amir does, every day.
More about Amir
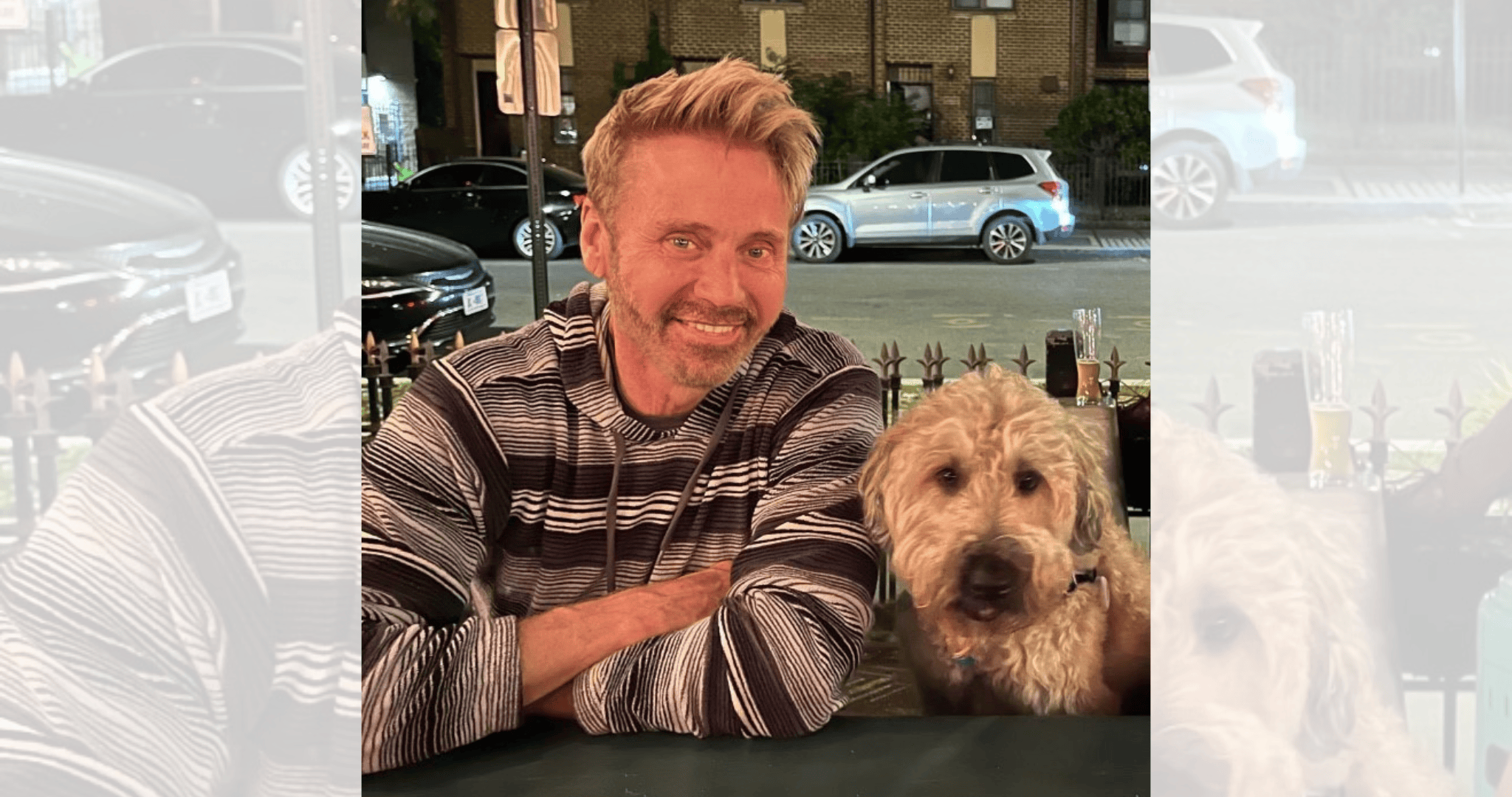
Amir Barzin ’06
Amir Barzin ’06 is the medical director for virtual care services and the UNC Clinical Contact Center for UNC Health.
After graduating from Carolina, Amir returned to his home state of Texas to complete a master’s in medical science and a doctor of osteopathic medicine degree at the University of North Texas Health Science Center. He then found his way back to Chapel Hill as a resident in the UNC School of Medicine’s Family Medicine Residency Program.
Since returning to North Carolina, Amir has also served as director of the UNC Family Medicine Center, a full-service primary care practice, and the chief resident physician of UNC Hospitals Department of Family Medicine.
To learn more about Amir Barzin ’06 and his work with the Carolina Together Testing Program, join his SEVEN Talk during the Morehead-Cain Alumni (Mini) Forum on Wednesday, November 17, at 4:00 p.m. ET. RSVP for the virtual event via the Morehead-Cain Network.
Connect with a mentor
The Morehead-Cain Mentoring Program is designed to leverage the power of the Morehead-Cain network by cultivating connections between scholars and alumni, and providing structure and support to these relationships so they can develop based on shared values and interests. All rising juniors and seniors are eligible to participate.
[quote text=”I’ve seen Amir’s example of intentionality and generosity in individual relationships cause a domino effect of inspired confidence and positive action in his communities.” name=”Frances Reed” year=”2022″ /]